Atlas Client Management
Streamlining client management
Role: Design Lead · Team: Health Solutions · Company: WW
WW Health Solutions partners with employers to propel happier, healthier, more engaged workplaces and communities.
How it works: WW memberships are offered at a discounted rate or are completely covered by an employer. In order to access the discounted membership rates, potential members must first go through the customized Health Solutions eligibility checkout flow.
Due to the complexity of determining eligible populations and legacy tech systems, a lot of the troubleshooting falls on the Health Solutions operations team to work with our clients in uploading, managing, and fixing member eligibility.
The current system is not scalable because it causes our team to have to do a lot of manual, repetitive, and tedious work due to systems not communicating with each other. This leads to inefficiency and frustration on our team as well as on the client side. In addition, it prevents us from being able to take on more or larger clients. I identified the user needs for the MVP below:
“Client admins don’t use this tool because they don’t find it helpful for troubleshooting errors. The information we see on the screen is basically a lie.”
Health Solutions Account Manager
Goal
Design a comprehensive tool to assist the team in optimizing client management processes.
Understanding our users
Operations
Our operations team is the main contact point for any issues relating to client population eligibility. They have to go through numerous channels in order to figure out what the problem is and how to solve it.
Account management
The account management team handles any client communication related to their contract with WW. It could range from engagement, contract negotiation, cost analysis, and troubleshooting member issues as well.
Client administrators
On the client side, they have admins that communicate directly with our WW operations and account management teams regarding anything about the partnership.
I conducted an audit of the current tooling being used in order to get a better understanding of what problems our team faces on a day to day basis.
I mapped out the current user flow by working with the operations team to go through their journey. It also allowed me to understand the underlying tech constraints that the engineers were trying to fix. It was important that we build the correct foundation this time around in order not to build up tech debt again and to ensure scalable processes and systems for the future.
Research & testing
User interviews
Before I began my design, I gathered information and data about the current problems in our system by interviewing a few Health Solutions teammates. This allowed me to ensure that we would be solving for the right user needs and creating the best experience possible.
Paper prototyping
To get clarity on the usability on my early design ideas, I designed a paper prototype of the desktop application to test whether or not the experience was intuitive, easy to learn, and solved our user needs.
Usability testing
Throughout my design process, I conducted numerous usability testing sessions to ensure that users and stakeholders were aware of the status of the project and to test the usability of the design. This helped me ensure that the design was constantly focused on the needs of the users.
Explorations
Final solution
Atlas portal
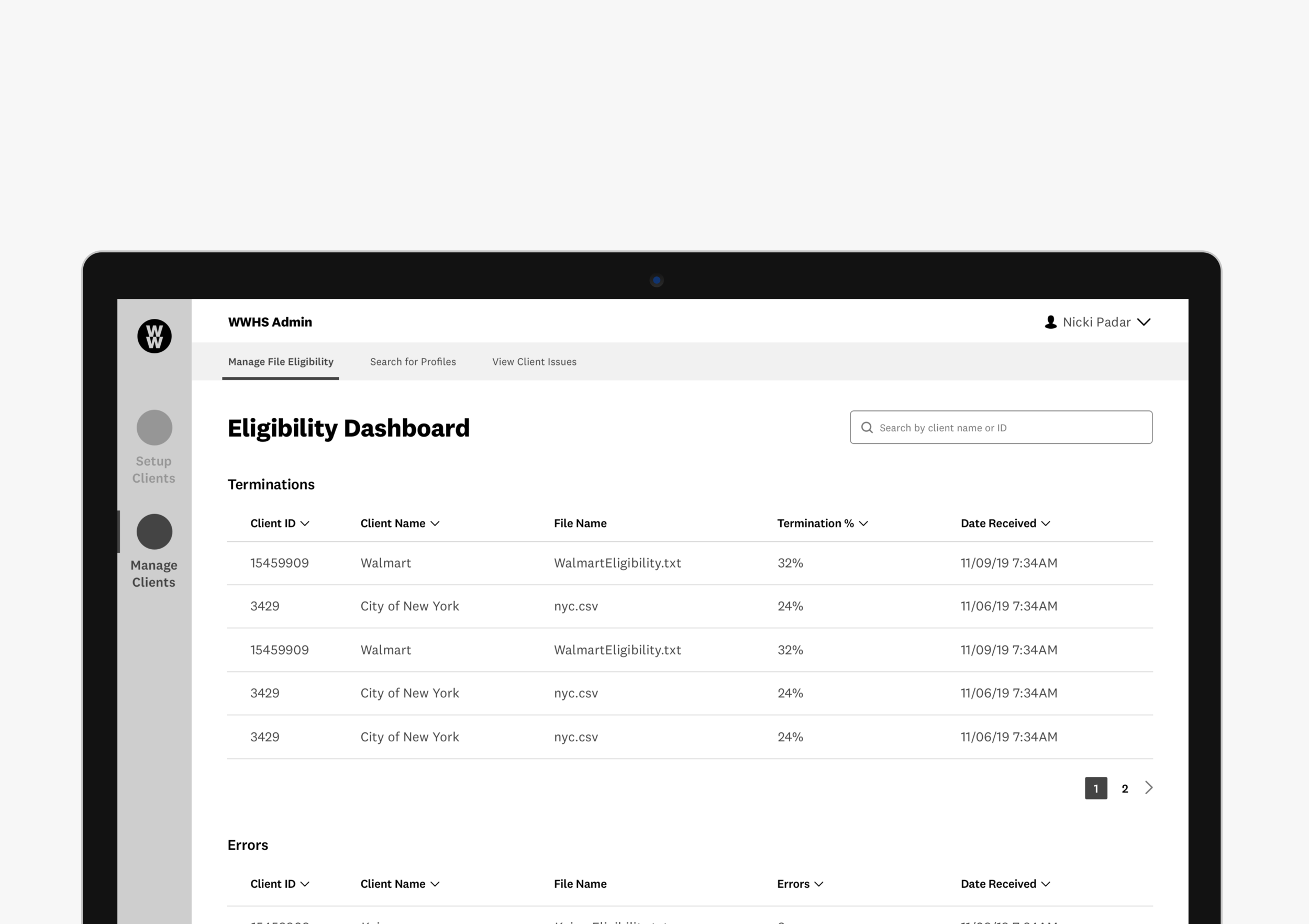
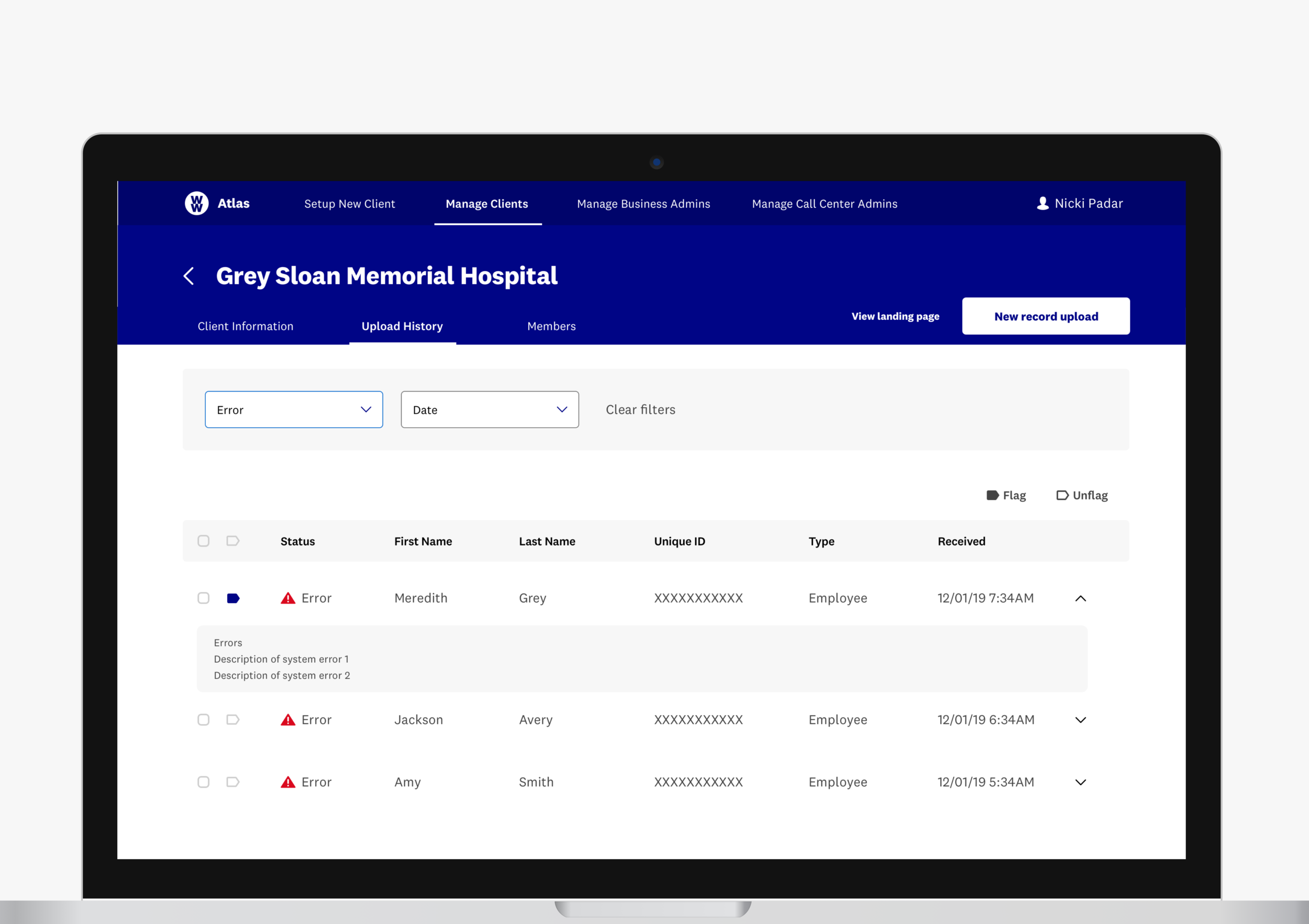
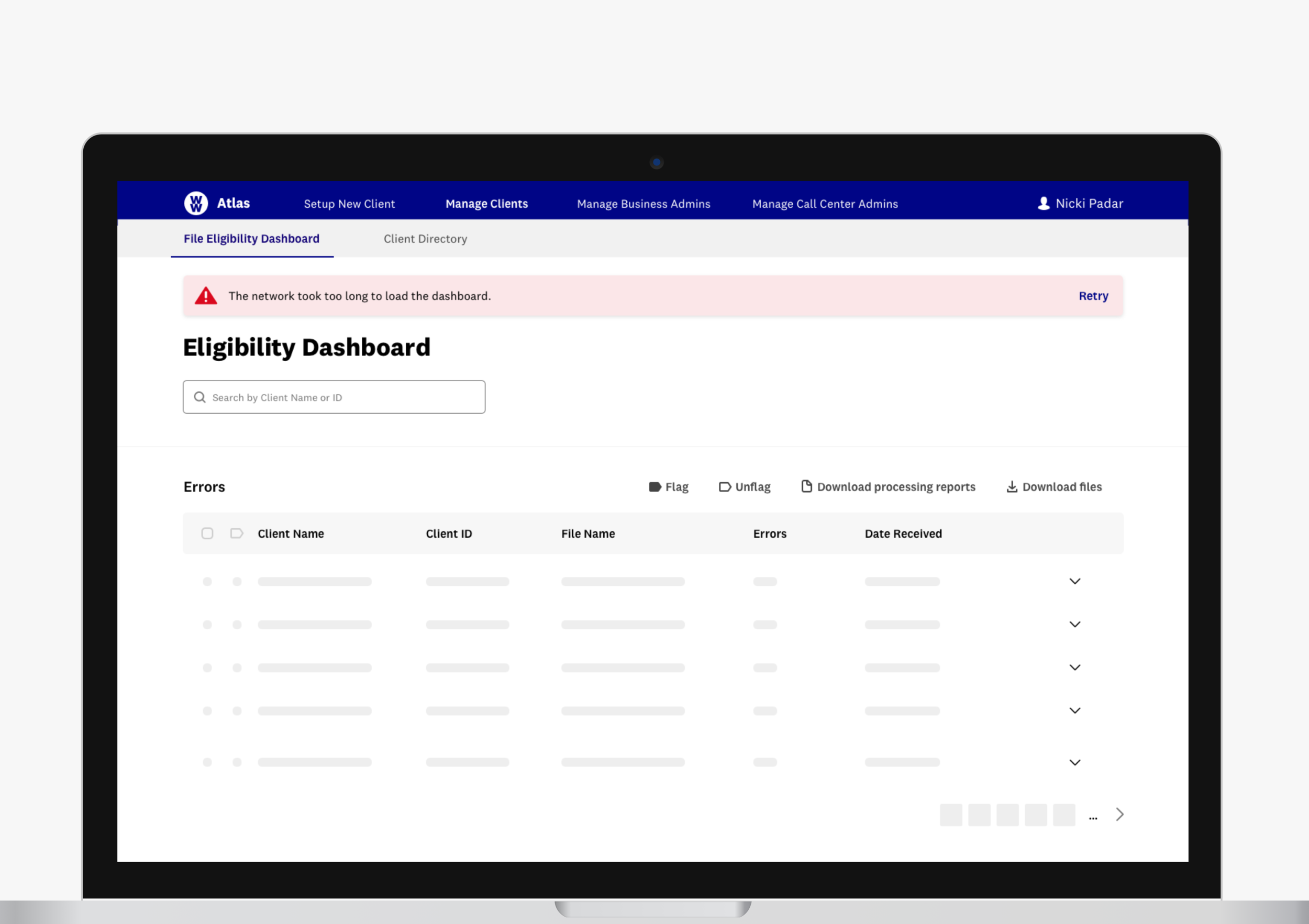
Eligibility dashboard
The dashboard is used to monitor and troubleshoot any client eligibility files that have errors or termination warnings. This helps the Operations team become more efficient in their day to day tasks by taking away numerous communication barriers between seeing what errors there are in the files and knowing who they should contact in order to fix it.
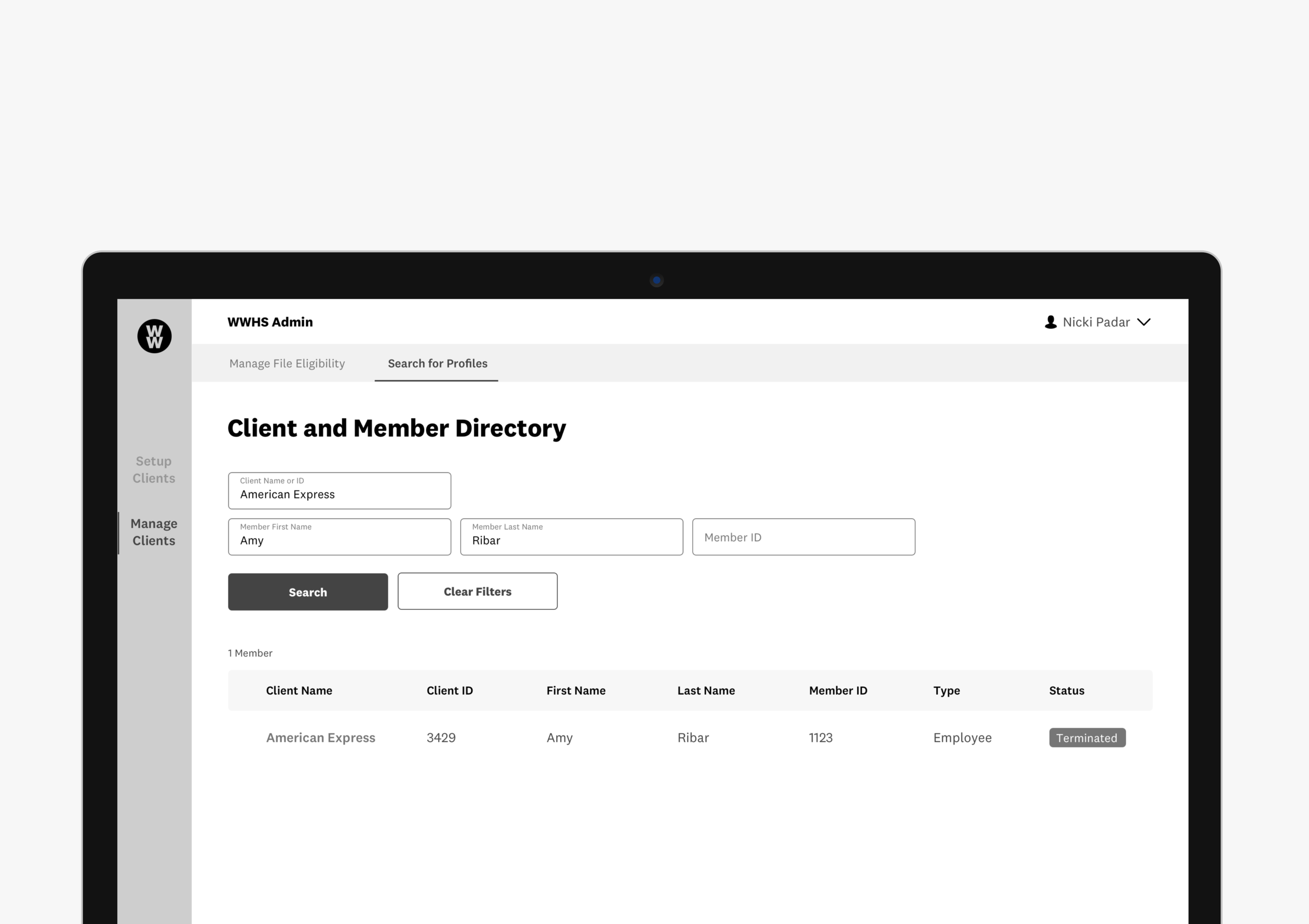
Search directory
This feature is a directory of all current and historical Health Solution clients, something that does not currently exist. This also includes any eligible lives within the clients population. This search functionality can tremendously improve workflows by providing a quick and easy way to find a specific client or eligible life.
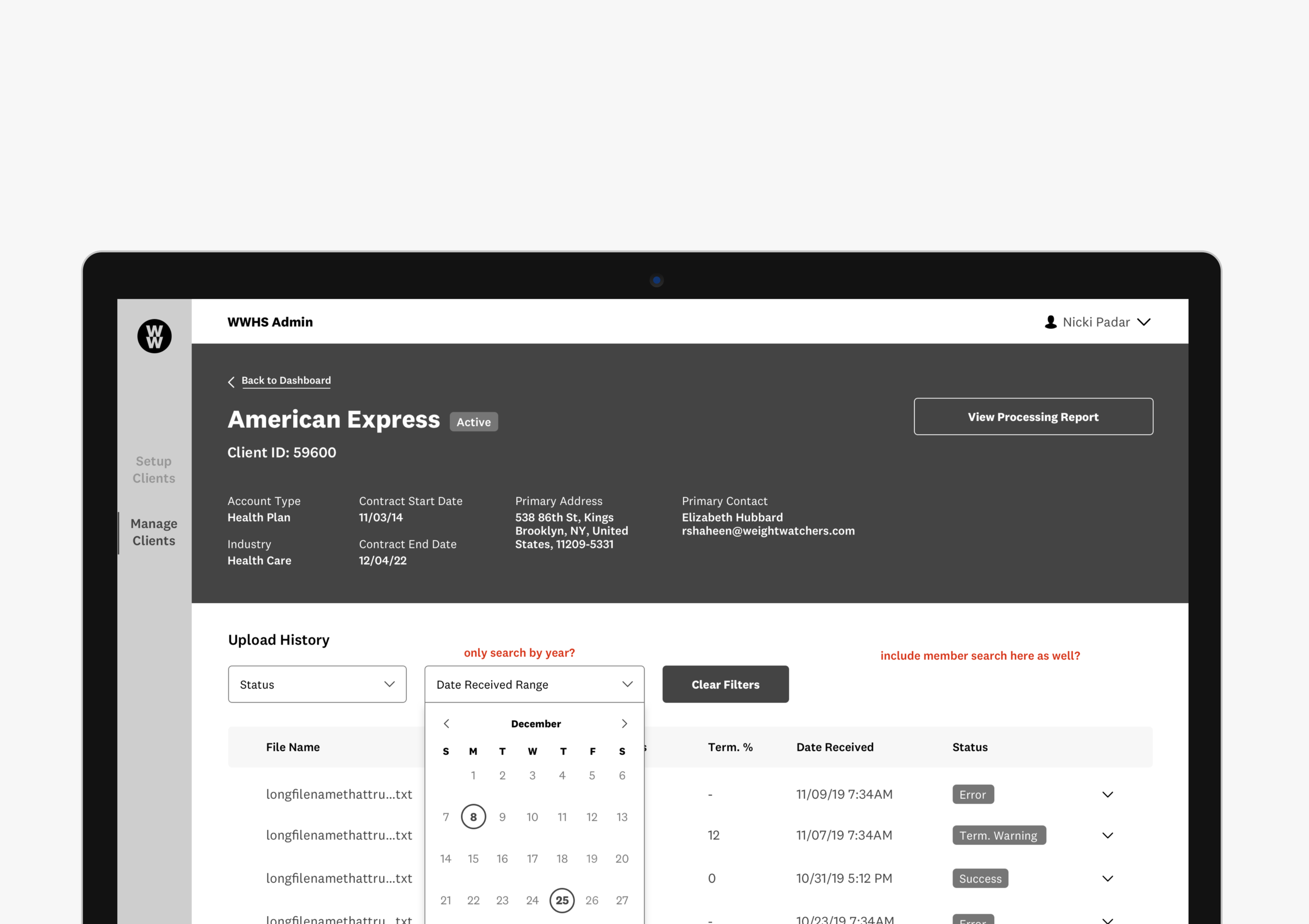
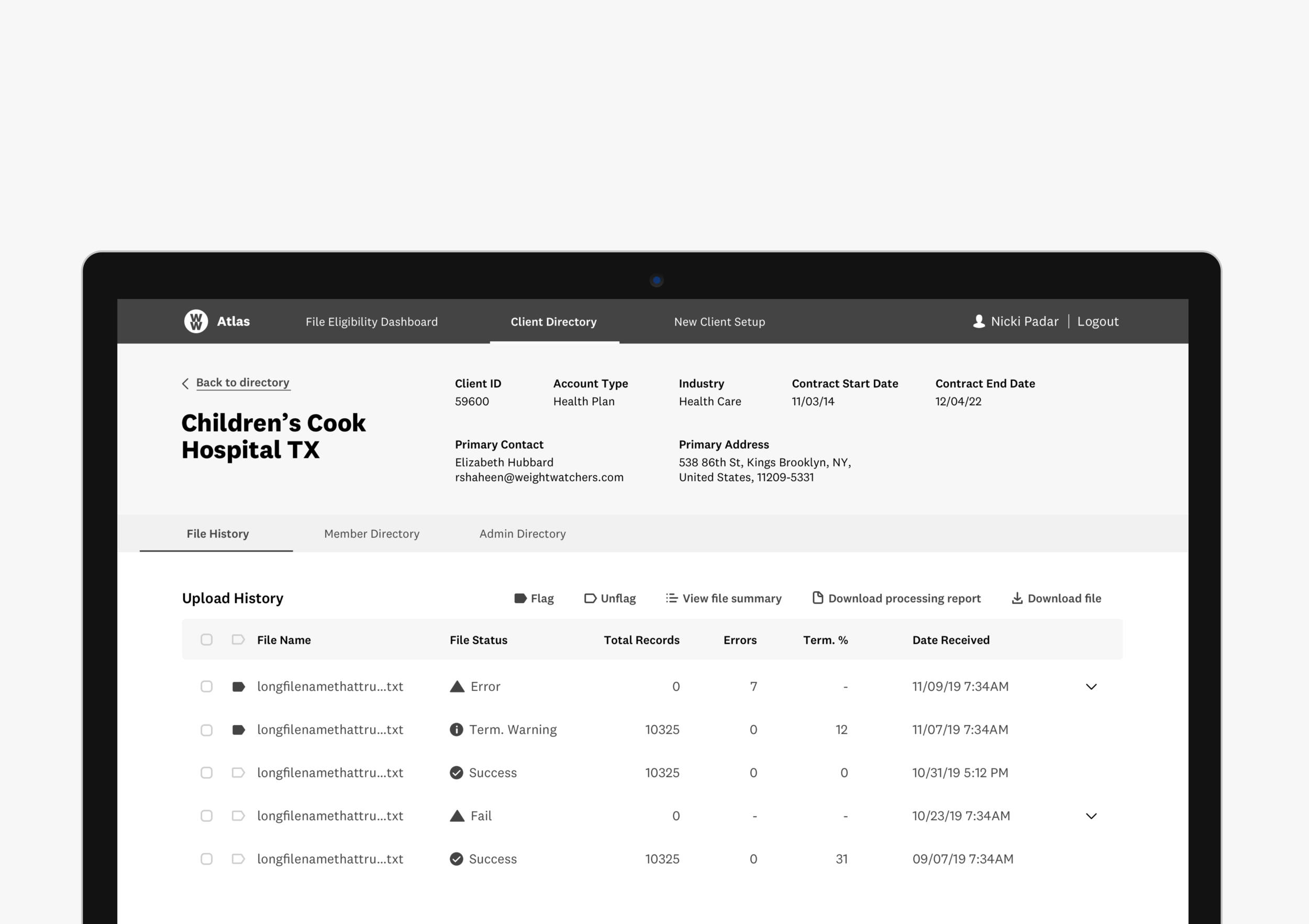
Client profile
This feature is used to store a specific client’s profile information and file eligibility history. Account management can then use this tool to do cost analysis with their clients in an efficient manner. It also provides historical data on a client, something that did not exist before. This data is useful to account managers when trying to troubleshoot eligible population status issues.
Admin settings
This feature allows the Operations team to add, delete, and update settings for business and client admins.
Metrics
Processes and communication between the team and their clients are improving
1 hour long calls are now 30 minutes
75% increase in efficiency when troubleshooting client issues
In addition, clients are now able to self troubleshoot, substantially decreasing our Ops teams need to intervene
Overall increase in team satisfaction
Improvements in the efficiency of onboarding new Operations and Account management team members.
“Our onboarding documentation for new team members used be 20 pages long with multiple training sessions. The training can now be done in one session with a two page document.”
Health Solutions Account Manager